
Hospitals under Pressure: Why 70 Extra Beds Are Only a Stopgap
Hospitals under Pressure: Why 70 Extra Beds Are Only a Stopgap
The Balearic authorities are providing more than 70 additional beds — Son Espases and Son Llàtzer are battling a flu wave. But the beds do not solve all problems. A reality check from daily life on the island.
Hospitals under Pressure: Why 70 Extra Beds Are Only a Stopgap
The facts are short and clear: This week the Balearic health authority is setting up more than 70 additional beds on the wards of Son Espases and Son Llàtzer, as covered in coverage of Son Llàtzer's response to the flu wave. Emergency departments are full of patients with influenza and other respiratory infections; at peak times nearly 80 people are waiting for a free bed. Some scheduled, non-urgent operations have been postponed.
Key question
Why are the additional beds not enough, and what consequences does the overload have for patients, staff and everyday life in Mallorca?
Critical analysis
More beds are important, but not equivalent to more care. A bed needs nursing staff, cleaning cycles, medication and diagnostics. When there are handovers in the emergency department and ambulances arrive outside with sirens, a prepared sea of stretchers helps little if there is no nurse to set up IVs or a doctor to write an admission. The data show: the cause is a combined wave of influenza and other respiratory infections — both increase short but intense peaks in emergency departments. This leads to longer stays, delayed discharges and therefore queues at the ward doors.
What is often missing from public debate
Four points are rarely mentioned. First: staff reserves. Beds can be set up faster than additional qualified staff can be recruited. Second: primary care and general practitioners. When patients with cough and fever go straight to the emergency department, additional pressure arises that outpatient care could better absorb. Third: transparency about the prioritization of postponed procedures — for those affected "postponed" is often not information but uncertainty. Fourth: prevention and vaccination rates. Information about the current flu vaccination campaign is often missing from public discussion — and this is a gap that could be closed with relatively little effort.
Everyday scene from Palma
An early evening at Son Espases: the car park half full, the automatic glass sliding door opens, a man with a scarf coughs into his sleeve, two young mothers push prams past. Inside you can hear the muted beeping of monitors through the corridors, voices in protective gowns, the sneezing of a waiting patient. In the cafeteria nurses quickly drink a hot coffee while the wind from the bay sweeps across the driveway. These small, recurring scenes show: people here are working at the limit of their capacity, not machines.
Concrete solutions
1) Short term: set up mobile transition units on wards — with clear protocols for prioritizing cases. These should be led by experienced nurses and have dedicated communication teams to inform relatives. 2) Strengthen outpatient shifts: better connect GP on-call services so that patients with uncomplicated respiratory infections go there instead of the emergency department. 3) Staff pools and recall mechanisms: return programs for retired or part-time staff, financial incentives for overtime during critical weeks. 4) Infection prevention and vaccination: an information campaign in pharmacies, schools and care homes; consider free or discounted flu vaccinations for risk groups. 5) Logistics: faster discharge management processes, more home care places and cooperation with private clinics to temporarily relieve bed pressure.
Practicality and limits
A field hospital may appear as a quick solution in other countries — on Mallorca space and personnel resources are limited. Every measure has costs and needs planning: recruiting staff cannot happen in weeks, vaccination campaigns need lead time, and relief through home care requires coordinated municipal structures. Still: combined, small measures can stabilize the system and prevent worse bottlenecks.
What island society can do
The most important thing locally is realistic expectation management. If you have a cough and fever, you should first contact your GP or the on-call service. Visitors in clinics should not contribute to the spread of infection through thoughtlessness. And: if you are eligible for vaccination, you should check available options — often a phone call to the nearest pharmacy or practice is enough.
Punchy conclusion
The 70 additional beds are a clear signal: the authorities are responding, and for a wider view see this analysis of Balearic clinics' preparations for the flu wave. But they are not a panacea. In the corridors of Son Espases and Son Llàtzer we see the interaction of beds, people and processes. If politicians, clinics and society only stare at bed numbers, they overlook the truly decisive levers: staff, outpatient services, transparent prioritization and prevention. In the short term beds help; in the medium and long term the island needs a coordinated strategy — otherwise the situation will be the same every year.
Date: 09.01.2026
Read, researched, and newly interpreted for you: Source
Similar News

Capdepera wants to curb rents — is the designation as a 'strained housing market' sufficient?
Capdepera has applied to be classified as a 'strained housing market' to enable rent controls. A necessary step, but not...

More hospital beds needed because of flu wave — a reality check
The Balearic health authority is installing more than 70 additional beds in Son Espases and Son Llàtzer. Why that helps ...
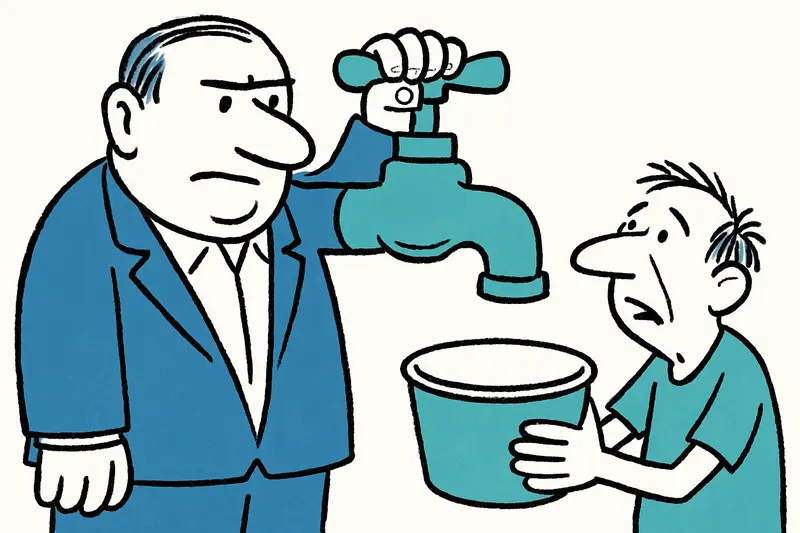
Son Fortuny: Whoever Buys the Estate Holds a Community at the Tap?
A huge estate in the Serra de Tramuntana is up for sale. It contains the only spring for a village — and the municipalit...
How a Wanted Man Was Caught in Binissalem — and What It Means for the Fight Against Online Fraud
A 44-year-old man wanted in Germany was arrested in Binissalem. The allegations: thousands of victims, scams via a paid ...

Arrest at Palma Airport: When an Open Car Becomes an Invitation
Police arrest at Palma Airport: A man is said to have searched several parked cars and stolen a vehicle after keys were ...
More to explore
Discover more interesting content

Experience Mallorca's Best Beaches and Coves with SUP and Snorkeling

Spanish Cooking Workshop in Mallorca
