
More hospital beds needed because of flu wave — a reality check
More hospital beds needed because of flu wave — a reality check
The Balearic health authority is installing more than 70 additional beds in Son Espases and Son Llàtzer. Why that helps in the short term but is not enough — a critical look from Mallorca.
More hospital beds needed because of flu wave — a reality check
Since 9 January 2026, hospitals on Mallorca have been visibly operating under high pressure: IB-Salut has registered more than 70 additional beds at Son Espases and Son Llàtzer because influenza and other respiratory infections are flooding emergency departments. At times almost 80 patients are waiting at the same time for a free bed; elective surgeries are being postponed. Those are the facts. The question is: Are additional beds enough to really solve the problem?
Clear guiding question
Are beds alone sufficient as a response to a seasonal wave of respiratory illnesses — or does Mallorca need a different, longer-term strategy that also considers staff, prevention and care processes?
Critical analysis
Beds on paper and beds in reality are two different things. A mattress, a monitor and an oxygen supply only help if there are enough nurses, doctors and diagnostic capacities available. The short-term increase in Son Espases and Son Llàtzer is likely to ease the worst bottlenecks: fewer people lying on stretchers in the corridor, faster transfers, a bit of breathing room for the emergency department. But: if staff are lacking or the beds cannot be sustainably staffed, the problem only shifts to other shifts and weeks.
In addition, queues of up to 80 people show that the care chain fails earlier — in clinics, in outpatient diagnostics, and in coordinating nursing homes. Unspectacular but dangerous: when patients remain in the emergency department for too long, the risk of nosocomial infections and chronic deterioration increases.
What is often missing in the public debate
The mere number of additional beds is often presented as a success. What is discussed less often: How are these beds staffed? Where do the short-term nursing and medical teams come from? Who ensures the supply of medication, oxygen and cleaning intervals? Structural questions are sometimes left out as well: How strained is primary care in Palma neighborhoods or in rural municipalities? Are prevention and vaccination offers being communicated in a targeted enough way?
A daily scene from Palma
Early in the morning in front of the entrance to Son Espases, a familiar, slightly worrying sight: a paramedic team pushes a stretcher into the waiting shelter where the wind passes the time. On the opposite side of the street a nurse pulls her coat tighter; she finished a night shift and quickly grabs a coffee from a kiosk on the avenue. Relatives sit wrapped up warm on the benches; someone is nervously on the phone. Rain taps quietly on the windshield of an ambulance. Such scenes are not only images; they are indicators of how everyday care is operating at the limit of its capacity.
Concrete approaches to solutions
If Mallorca does not want to go into alarm mode every year during an infection wave, measures must interlock. In the short term, additional beds help — but only together with:
1) Staffing strategy: Short-term deployments of specialists from less burdened regions, simplified procedures for extending shifts with compensation, but above all a medium- to long-term plan for training and retaining nursing staff in the Balearic Islands.
2) Outpatient relief: Extended opening hours for general practitioner practices during the season of high respiratory infections, mobile clinic teams that specifically visit nursing homes and assisted living communities.
3) Prevention and communication: Local vaccination campaigns with easily accessible offers (marketplaces, municipalities), clear communication about which symptoms warrant a visit to the emergency department and when the family doctor is sufficient.
4) Coordination between hospitals and social services: Faster transfer rules, more short-term care places as a bridge after hospital stays, coordinated protocols with private clinics that can free up capacity.
5) Temporary infrastructure: Quickly erected treatment zones outside the main buildings (modular units, heated tents) to reduce infection risks in emergency departments and triage patients more rapidly.
What we can do locally
As neighbors, employees, a small practice or a municipality, people can contribute: actively reach out to risk groups, communicate vaccination appointments transparently, mobilize volunteer drivers for transport services and involve volunteer organizations. Small measures at the municipal level reduce the burden on emergency departments in the medium term.
Pithy conclusion
The additional 70 beds at Son Espases and Son Llàtzer are right and necessary — but they are not a panacea. Without staff, outpatient relief and coordinated prevention, the island remains vulnerable every winter. Mallorca now needs an honest discussion about resources, not just bed numbers: where is staff missing, how are vaccination offers organized and who ensures coordinated follow-up care? Short-term relief yes, real change preferably yesterday rather than tomorrow.
Read, researched, and newly interpreted for you: Source
Similar News

Capdepera wants to curb rents — is the designation as a 'strained housing market' sufficient?
Capdepera has applied to be classified as a 'strained housing market' to enable rent controls. A necessary step, but not...
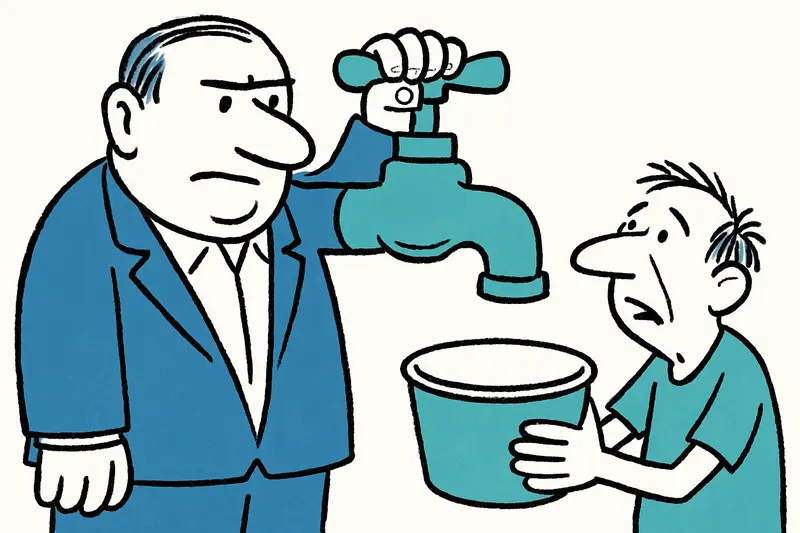
Son Fortuny: Whoever Buys the Estate Holds a Community at the Tap?
A huge estate in the Serra de Tramuntana is up for sale. It contains the only spring for a village — and the municipalit...
How a Wanted Man Was Caught in Binissalem — and What It Means for the Fight Against Online Fraud
A 44-year-old man wanted in Germany was arrested in Binissalem. The allegations: thousands of victims, scams via a paid ...

Arrest at Palma Airport: When an Open Car Becomes an Invitation
Police arrest at Palma Airport: A man is said to have searched several parked cars and stolen a vehicle after keys were ...

E-Scooters: Online Register Coming — Who Will Check Insurances in Mallorca?
The Spanish government plans a nationwide online register for e-scooters. But what does this mean for users in Mallorca,...
More to explore
Discover more interesting content

Experience Mallorca's Best Beaches and Coves with SUP and Snorkeling

Spanish Cooking Workshop in Mallorca
